
Lumbar osteochondrosis is a dangerous disease of the spine, characteristic of people who have reached the age of 35 years or older. The natural wear and tear of joints causes the development of pathology. Early access to a rheumatologist, in most cases, leads to disability. Modern medicine offers many effective methods of treatment in the early stages. Early diagnosis is the key to a healthy life without restrictions.
Lumbar osteochondrosis - general definition
Osteochondrosis of the lumbar spine is a process of dystrophic degeneration in the formations of intervertebral cartilage - discs.
Discs provide the main functions of the spine - the ability to move and bend, resistance to stress. As a result of pathology, important elements become thinner, deformed, vertebrae are aligned, nerve endings and blood vessels are compressed. Negative processes are accompanied by painful sensations of varying intensity and limitation of motor function.
The pathology causes changes in the connecting elements of the spine - cartilage, bones, discs and joints. It is caused both by natural processes of wear and tear and by acquired joint disease or the result of an inappropriate lifestyle.

Causes
There can be many reasons for the development of lumbar osteochondrosis:
- Natural or premature wear of the body;
- Excessive load on the lower back - lifting loads, working "standing" or a sedentary and "sedentary" lifestyle;
- Genetic predisposition to joint diseases such as rheumatoid arthritis;
- Violation of metabolism, resulting in the accumulation of toxic substances in the connecting discs;
- Chronic diseases of the circulatory system. Nutrients and trace elements fail to enter the cartilage tissue in adequate amounts. Hypoxia sets in, which contributes to the destruction of intervertebral joints;
- Autoimmune pathologies.
Secondary factors can also provoke the development of lumbar osteochondrosis:
- Chronic injuries, back bruises;
- Exceed the weight norm by more than 15-20%;
- Heavy or strength sports;
- Constantly wearing uncomfortable shoes. High heels, tight shoes, rubber or sports shoes are the spine's first enemies;
- Valgus changes in the foot;
- Scoliosis, kyphosis, diabetes mellitus, spinal tuberculosis;
- Impact of low temperatures.
Clinical condition
The symptoms of lumbar osteochondrosis completely depend on which nerve roots are affected by the disease. The degree of compression of the vertebrae, the stage of the disease, and disc damage determine the signs.
Rheumatologists distinguish the following main symptoms:
- Violation of tactile susceptibility in the lumbar region. The numbness extends to the inner thighs and groin. It can affect one or both members;
- There is a sharp, sharp pain in the lower back. The big toe completely loses mobility and characteristic numbness is observed;
- Loss of normal foot function, sensation of toes, lower leg and outer thigh. In these parts of the leg, there is a regular tone and convulsive attacks. On examination, there is no Achilles reflex;
- If the disease affects the inferior radicular artery, there will be complete paralysis of the muscles of the buttocks, back of the thighs and perineum. There is a serious violation of motor function, up to complete immobility.
With lumbar osteochondrosis, not only the nerve endings in the spine are affected, but also the blood vessels.
The following specific signs depend on the type of injury:
- When only the nerve roots are disturbed, a change in the patient's gait is observed. The pain is located not only in the lower back, but also in all parts of the legs. The radicular syndrome is characterized by constant pain. Usually only on one side. In the lower back, tingling and aches are noticed. Pain can be relieved with a little exercise.
- Compression of blood vessels leads to perfusion in the hip area. As a result, there is a lack of oxygen from the spinal discs. Painful sensations occur when walking on the buttocks, thighs and lower back. Completely removed after a night's rest.
Simultaneous violation of the functionality of blood vessels and nerve roots can lead to irreversible deformation of the discs. Spine-like bony outgrowths form on the movable joints of the lower back. This leads to intense pain and makes normal natural movement impossible. Violated posture, gait. As it progresses, complete paralysis can occur.
stages of the disease
Lumbar osteochondrosis develops gradually, in several stages. Each stage has its own characteristics, which determine the degree of progress.
- I stage.Slow destruction of the intervertebral discs begins. The process can last from several months to 2-5 years. It is manifested by minor pain, discomfort in the inguinal and femoral muscles. It is noticed when walking or when the weather changes.
- II stage. Collagen fibers from the fibrous rings of the spine are attracted to the negative process. The space between individual vertebrae is rapidly shrinking. Friction appears, which causes severe attacks of pain. Violated gait, posture, tilt appears. Lumbar osteochondrosis is most often diagnosed in the second phase of the course.
- III stage.An intervertebral hernia appears. And if the patient has not been forced to seek medical help with stage II symptoms, it will no longer be possible to ignore the excruciating pains of stage three. The deformation of the bones and joints of the spine in the lumbar area is already irreversible. Walking takes a lot of effort. This is due to the pain and the inability to relieve it with conventional painkillers.
- Step IV.Partial or complete impairment of motor function. At this stage, the patient is assigned to a disability group. Threaten with complete paralysis. Vital activity is impossible without taking a wide range of medications.

diagnostic measures
Diagnostic measures include several techniques and begin with taking a complete history of the disease. During the initial consultation with a rheumatologist, the following data are clarified:
- The patient's complaints are carefully analyzed - the location of the pain, where the discomfort is still felt, in which parts of the hip joint there is a feeling of heaviness, convulsions, etc. ;
- Duration, regularity, nature of pain;
- When the first symptoms, even minor ones, appeared. How much time has passed since the last attack, what causes discomfort and what factors contribute to its elimination;
- Surrounding living conditions of the patient. Profession, work, household workload, sports and the presence of additional factors for increased physical activity (dacha, gardening, hobbies associated with weight transfer);
- Examination of the history of illnesses that the patient has suffered in the past or present.
After collecting the clinical picture, the rheumatologist proceeds directly to the external examination. During the examination, the gait, the anatomical position of the legs, arms, trunk, in relation to the spine are analyzed. The skin is examined for changes - pigmentation, scaling, eczema, rashes, etc. An assessment of motor function is given.
Performing simple exercises - leaning forward, backward, lifting arms and legs, turning the head, rotational movements of the pelvis, the patient allows the doctor to determine the degree of damage to the spine in the lower back.
The final measurements of the external examination are actions to determine the degree of root damage:
- Lasegue symptom.Lying on the back, the patient raises the legs alternately, bent at the knee. If this causes pain in the lower back, the readings are considered positive.
- Dejerine symptom.The patient is asked to tighten the abdominal muscles as much as possible. The occurrence of discomfort in the spine indicates the development of lumbar osteochondrosis.
- Neri Symptom. Sharp forward and backward head tilts respond with pain in the lower back.
- Wasserman symptom. The patient, in the supine position, moves the leg as far as possible to the side. In the presence of pathology, unpleasant pain occurs in the groin and front of the thigh.
To confirm or exclude the diagnosis, the patient is asked to undergo instrumental diagnosis. MRI is considered the most effective way to determine lumbar osteochondrosis. The study shows the distance between the vertebrae, the development of neoplasms and bone deformities. It may be contraindicated in patients with mental disorders.
Computed tomography provides a fairly true picture of the disease in one plane - either horizontally or vertically.
X-rays are only used in the later stages, when irreversible changes in the bone tissue of the spine begin.

Complex treatment of lumbar osteochondrosis
The causes of the pathology have not been fully elucidated. Scientific research in the field of spinal joint diseases has not yet identified sufficiently effective methods for the complete restoration of intervertebral discs. Modern methods of treatment are aimed only at eliminating the external signs of the disease. Full recovery is currently considered impossible.
traditional drug therapy
The rheumatologist prescribes medication depending on the general condition of the patient. The clinical picture provides the necessary information for the elaboration of a therapeutic regimen with drugs from different groups.
- anesthetic agents.Injections, ointments, or broad-spectrum medications are prescribed.
- Anti-inflammatory drugs (NSAIDs).
- Vasodilators.Removal of tone from the muscles of the lower back and legs.
- Chondroprotectors.Designed to exclude the negative progress of lumbar osteochondrosis.
Physiotherapy
Physiotherapy procedures are an integral part of inpatient or outpatient treatment of lumbar osteochondrosis.
It includes the following activities:
- Electrophoresis with analgesics;
- Magnetotherapy;
- Hydrotherapy;
- Paraffin applications.
Medications and physical therapy in the complex relieve acute pain and inflammation. But they are not a guarantee of stopping the progress of the pathology. Just a course of treatment 2-3 times a year and a responsible attitude of the patient will help to avoid regression and maintain the general condition satisfactorily.
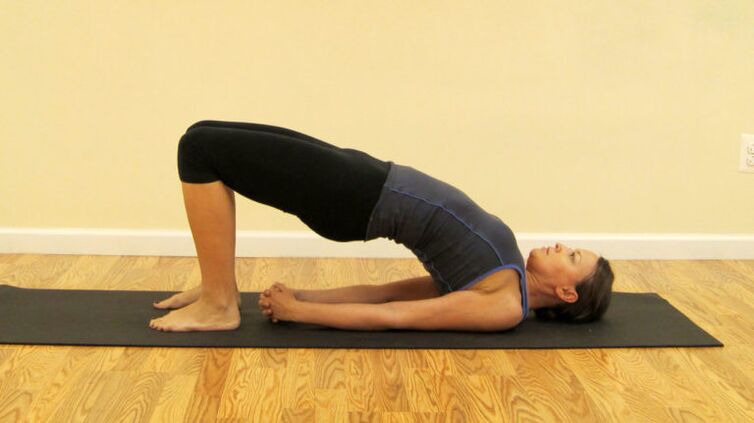
Exercise therapy and massage therapy
A set of therapeutic gymnastics exercises ensures the normalization of blood circulation in the lower back and helps to eliminate stagnant processes. Only a physical therapist can prescribe exercises for clinical or home use. As a rule, it's all sorts of gentle bending and rotational movements, from a prone position to a sitting position. Independent physical activity may not only bring results, but cause even more displacement of the vertebral discs.
Manual therapy sessions help to strengthen muscle tissue, blood flow to the affected lower back and relieve tension. The specialist massages a healthy part of the back first, to warm the muscles and improve blood circulation. Then it goes to the affected areas of the lower back. The manipulation area includes the lower back, buttocks, thighs, shins and feet. Sessions are held in regular courses, at least 10 sessions in 6 months.
Surgical intervention
It is indicated in the last stage of lumbar osteochondrosis, with the aim of restoring the motor function of the spine. Surgery remains the only option for patients who experience the following symptoms:
- Constant pain syndrome, untreatable even with opiate-containing drugs;
- Strong compression of the nerve roots and significant displacement of the discs;
- Neoplasms, proliferation of bone tissue;
- Complete destruction of the vertebrae, due to constant friction;
- Paralysis.
Modern methods offer less traumatic methods of internal intervention. For example, endoscopy. It has a favorable prognosis, short period of rehabilitation and low rate of side effects.

Alternative treatment
Lumbar osteochondrosis responds well to treatment with medicinal herbs and folk methods. Ointments, tinctures, fee-based baths are used to relieve swelling and pain. The most effective recipes include anesthetic and anti-inflammatory herbs:
- yarrow;
- aloes;
- Pepper mint;
- Saint John's herb;
- spruce or pine needles;
- Wise.
The content of these herbs in popular recipes is due to their medicinal effects, scientifically proven by traditional medicine. Home treatment will help keep the lower back in a stable condition and prevent the disease from exacerbating after complex treatment.
Prevention
Although lumbar osteochondrosis is an incurable disease, its negative manifestations can be minimized. In the early stages, the disease is successfully treated, it is only necessary to seek medical help in a timely manner. It is important to adhere fully to the treatment regimen designed and to follow the rheumatologist's recommendations.



















